The concept of self-medicating often arises when individuals attempt to manage their physical or emotional pain using legal or illicit substances, such as alcohol, prescription medications, or recreational drugs. This behavior may stem from a desire to numb distressing emotions, cope with ongoing stress, or avoid confronting underlying mental health issues.
While it might provide a fleeting sense of relief or control, self-medicating can mask symptoms rather than address their root causes, ultimately intensifying the very problems it seeks to ease. Over time, this approach increases the likelihood of substance dependence and addiction, creating a cycle that becomes increasingly difficult to break without professional help.
The consequences can extend beyond the individual, affecting relationships, work performance, and overall well-being. This article examines self-medicating behaviors in depth, explores the short- and long-term risks involved, and offers insight into effective strategies for breaking the cycle and moving toward lasting recovery.

Exploring Self-Medicating Behaviors
Definition and Purpose
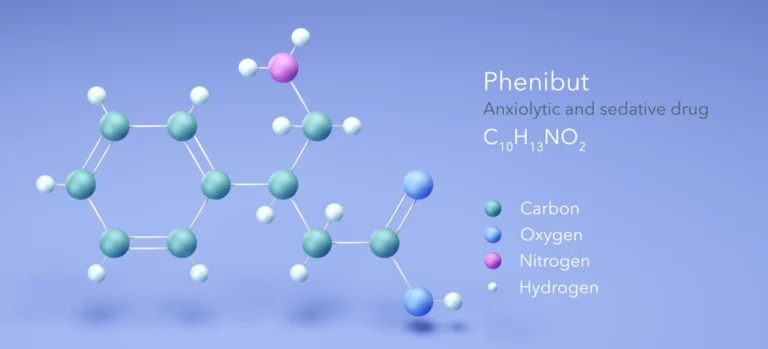
Self-medicating involves using drugs or alcohol without medical supervision to alleviate symptoms of mental health disorders or physical pain. Individuals often turn to this approach as a coping mechanism for anxiety, depression, or trauma, attempting to manage overwhelming emotions on their own.
While the choice to self-medicate may arise from a sense of desperation or a lack of access to proper care, it can also be influenced by cultural attitudes toward substance use, stigma surrounding mental health treatment, or misinformation about the safety of certain drugs.
In some cases, people may not even recognize that their behavior qualifies as self-medicating, particularly if the substances used are legal or socially accepted. Over time, this reliance can blur the line between casual use and dependency, increasing vulnerability to harmful patterns that become harder to reverse without intervention.
Reasons Behind Self-Medicating
Emotional Pain Relief
Many individuals self-medicate to numb emotional pain, escaping temporarily from anxiety, depression, or stress. In some cases, inaccessible or costly healthcare drives people to find alternative solutions for pain management, leading to substance misuse.
Social influences, such as peer pressure, family modeling of unhealthy coping habits, or exposure to environments where substance use is normalized, can further reinforce these behaviors. A lack of awareness about healthier coping strategies or available support systems may leave individuals feeling trapped, with substances appearing to be the most immediate or familiar option.
Over time, what begins as an attempt to gain a sense of control over distress can evolve into a dependency that erodes mental, physical, and emotional well-being, making professional help both more necessary and more challenging to seek.

Risks Associated with Self-Medicating
Progression to Addiction
Regular self-medication can lead to tolerance, where the body increasingly requires higher doses of a substance to achieve the desired relief or effect. This escalation not only raises the risk of overdose but also places significant strain on the body’s organs and overall health. Over time, individuals may develop physical dependence, experiencing withdrawal symptoms when the substance is not present, or psychological dependence, where cravings and compulsive use dominate their thoughts and behaviors.
What initially seems like a helpful coping mechanism gradually becomes a central focus in a person’s life, often overshadowing other healthy ways of managing emotions or pain. Moreover, the continued use of substances can interfere with brain chemistry, worsening anxiety, depression, or other mental health conditions and making recovery more complex.
This creates a vicious cycle in which attempts to alleviate discomfort inadvertently deepen both physical addiction and psychological distress, making it increasingly difficult to break free without comprehensive treatment and support.
Health and Social Consequences
Prolonged substance misuse can cause severe health issues, including liver damage, heart problems, and neurological impairments. Beyond the physical toll, chronic use of substances often weakens the immune system, making individuals more susceptible to infections and other medical complications.
Cognitive functions such as memory, attention, and decision-making may also decline, affecting daily life and long-term prospects. Substance dependence frequently leads to strained relationships, impacting family dynamics and social networks. Trust can erode as loved ones witness unpredictable behaviors, mood swings, or broken promises, often leading to feelings of isolation and loneliness for the individual struggling with addiction.
Social withdrawal is common, as individuals may distance themselves from friends and community to hide their use or avoid judgment. Additionally, financial difficulties stemming from the cost of sustaining an addiction can exacerbate tensions within families and contribute to unstable living situations, further complicating recovery efforts.

Addressing Substance Dependence in Knoxville, TN
Local Treatment Options
Facilities like the Knoxville Recovery Center offer specialized programs designed to address the complex needs of individuals struggling with substance dependence. These programs typically integrate comprehensive medical treatment, including detoxification and medication-assisted therapies, alongside psychological support such as individual counseling, cognitive-behavioral therapy, and trauma-informed care.
By combining these approaches, the center aims to treat not just the addiction itself but also the underlying mental health issues that often accompany it. In addition to inpatient and outpatient services, Knoxville Recovery Center provides access to various community-based support groups, peer mentorship programs, and holistic therapy options like art therapy, mindfulness practices, and exercise-based interventions.
These resources work together to create a supportive environment that encourages sustained recovery, helps individuals develop healthy coping skills, and reduces the risk of relapse. The emphasis on a personalized treatment plan ensures that each person receives care tailored to their unique circumstances, fostering empowerment and hope throughout their journey toward long-term wellness.
Holistic Recovery Approaches
Integrating medical, psychological, and social support ensures a rounded and comprehensive approach to recovery, effectively addressing the root causes of self-medicating behaviors rather than just the symptoms.
This multifaceted method recognizes that addiction is often intertwined with various aspects of a person’s life—including mental health challenges, social environments, and personal histories—requiring treatment plans that are adaptable and holistic.
Alongside direct clinical interventions, educational initiatives play a crucial role in raising public awareness about the risks and consequences of self-medication, helping to dispel common misconceptions and reduce stigma around seeking help. These programs often focus on teaching practical skills for stress management, emotional regulation, and problem-solving, empowering individuals to replace harmful behaviors with healthier coping mechanisms.
Community outreach and school-based education further contribute to prevention by targeting at-risk populations early, fostering resilience and informed decision-making. Ultimately, this integrated approach not only supports sustained recovery but also promotes long-term wellness by equipping individuals and communities with the knowledge and resources needed to prevent relapse and encourage healthier lifestyles.
FAQs About Self-Medicating and Addiction
What are the signs that someone is self-medicating?
Signs of self-medicating include increased substance use during periods of heightened stress, using drugs or alcohol specifically as a way to cope with difficult emotions such as sadness, anger, or loneliness, and neglecting important personal, professional, or social responsibilities due to substance use.
Other indicators may involve changes in behavior or mood, such as irritability, withdrawal from previously enjoyed activities, or secretive actions to conceal the extent of use. Individuals may also experience physical symptoms like fatigue, changes in appetite, or unexplained health issues that correlate with their substance use patterns.
Additionally, self-medicating often leads to a growing preoccupation with obtaining and using substances, which can interfere with the ability to focus, make decisions, or maintain healthy relationships. Friends and family might notice fluctuations in performance at work or school, increased absenteeism, or an overall decline in functioning, which can serve as warning signs that someone is relying on substances to manage underlying emotional or psychological struggles.
How can self-medicating lead to addiction?
Self-medicating can lead to addiction as individuals gradually develop tolerance, requiring increasingly larger amounts of a substance over time to achieve the same desired effects. This escalating use often results in physical and psychological dependence, where the body and mind begin to rely on the substance to function normally.
As tolerance builds, what once started as occasional or controlled use can spiral into compulsive behavior, with the individual losing the ability to regulate or limit their consumption. This loss of control is a hallmark of addiction and can profoundly impact daily life, as the drive to use substances overrides other priorities and responsibilities.
Moreover, addiction fueled by self-medication often brings about significant changes in brain chemistry, reinforcing cravings and making it more difficult to quit without professional intervention. The cycle becomes self-perpetuating: increased use leads to more dependence, which in turn deepens the addiction, creating barriers to recovery and increasing the risk of severe health, social, and emotional consequences.
What steps can one take to stop self-medicating?
Seeking professional help is a vital step in overcoming self-medicating behaviors and the resulting addiction. This process often involves a combination of therapy, such as cognitive-behavioral therapy or trauma-informed counseling, alongside medical treatments like detoxification and medication-assisted therapy to safely manage withdrawal symptoms and underlying health conditions.
In addition to these clinical interventions, joining support groups provides a sense of community and shared understanding, allowing individuals to connect with others who face similar challenges and gain encouragement through mutual experiences.
Beyond formal treatment, developing healthy coping mechanisms is essential for long-term recovery; this might include practices such as mindfulness, stress management techniques, regular physical activity, creative outlets, or building strong daily routines that foster emotional resilience.
Equally important is cultivating a supportive environment—whether through family, friends, or peer networks—that offers accountability, compassion, and motivation. Together, these elements create a foundation that empowers individuals not only to break free from substance dependence but also to rebuild their lives with greater balance, purpose, and well-being.

Moving Beyond Self-Medication
Understanding the potential dangers of self-medicating is the first step toward seeking healthier solutions for pain management and emotional distress. Addressing these behaviors through professional support and robust recovery plans can pave the way to overcoming addiction and restoring well-being. If you or someone you know is struggling with self-medicating behaviors, contact the Knoxville Recovery Center for expert guidance and comprehensive care, or call us at 865-830-3967 to learn more about available recovery options.